Interstate medical licensure compacts (IMLC) are an expedited process for clinicians to obtain license credentials when seeking to practice their trade in multiple states. Originally, it was designed to doctors, but today the same process also applies to nurses and physical therapists. The practice has been praised as a way to help alleviate knowledge worker shortages by allowing clinicians to take on locum, temporary, or permanent assignments in other states without the hassle of traditional licensure. The side effect has been an increase in the number of doctors able to practice telehealth across state boundaries.
Let’s look at the pros and cons of the IMLC and whether it could benefit the field of telemedicine. What other unexpected outcomes could the IMLC bring about?
Understanding the Goals of the IMLC
 Making it easier to obtain licensure across state lines is just one of the goals of the IMLC. Because there is no consistent nationwide licensure process, the IMLC stepped up to attempt to provide license portability between states. It should be noted that this voluntary collaboration between state medical and osteopathic licensing boards is not tied to federal regulatory bodies. The IMLC website says, “The Compact is of the states, by the states and for the states.”
Making it easier to obtain licensure across state lines is just one of the goals of the IMLC. Because there is no consistent nationwide licensure process, the IMLC stepped up to attempt to provide license portability between states. It should be noted that this voluntary collaboration between state medical and osteopathic licensing boards is not tied to federal regulatory bodies. The IMLC website says, “The Compact is of the states, by the states and for the states.”
The Compact came about in 2013, when state medical board executives, attorneys, and healthcare administrators come together to create the first licensure agreement. The IMLC isn’t owned by one entity; instead, a Board of Directors made up of two representatives from each Compact state governs the organization.
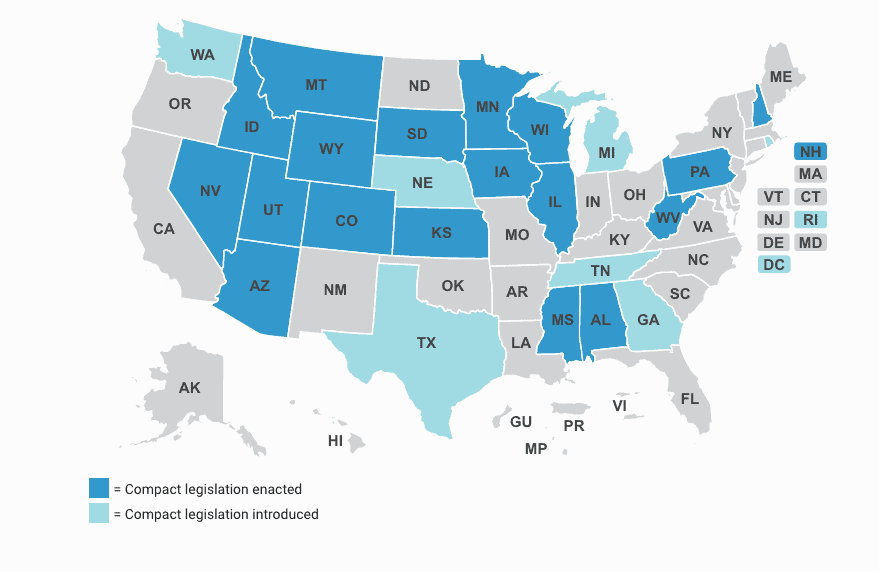
Any doctor from a state participating in the Compact, that meets stringent qualifications from the IMLC, can apply for a multi-state licensure. The doctor can only be licensed in the states participating in the Compact. Today, that is one-half of all the states in the U.S.A. – and that number is predicted to climb.
States can sign up for the IMLC via a legal agreement that defines the interstate licensing of clinicians. The state legislature and Governor must sign off on the new rule and the Compact language must be the same in every state.
Lawyers Kendall & Davis suggest that the IMLC does more than extend the licensure of participating clinicians, but that the IMLC was seeking a way to “standardize the safety and security of licensure, and by extension, patient care, across all states.”
How does it Work?
Physicians must apply through the IMLC after meeting requirements*, including:
- They must already be licenses in a participating Compact Member State.
- Must have a spotless record of care delivery.
- The physician must choose a primary State of Principal License (SPL).
The physician’s background credentials and legal history are reviewed and the Commission determines whether they can receive licensure. All of these states are supposed to share complaint/investigative information so that if the physician comes under review in one state, all states will take similar action. It is in this way that the IMLC will fulfill its goals of improving patient safety via the licensure compact.
*Summary of requirements list. For the full list of requirements, click here.
What are the Barriers?
A number of problems still stymie our efforts to provide telehealth across state lines. One of the barriers currently, is that clinicians are in effect double-billed for their license. According to Kendall & Davis, there is a $700 licensure fee paid to the IMLC plus each state requires a similar fee to apply.
To date, true portability between states has not been achieved, so physicians practicing in multiple states must adhere to state-specific practice regulations. They must also pay annual state-specific license renewal fees. Shirley Svorny, a Professor of Economics at California State University suggests that the Compact doesn’t go far enough, stating, “The Compact continues the problematic arrangement in which multiple boards license the same physicians.” She continues, “The compact is a missed opportunity for this country as the benefits to patients of license portability would be substantial.”
Too, the FBI has given some pushback on conducting criminal background checks without additional specific wording to their state Compact rules. To date, many states have revised their Compact language to include FBI requirements so that background checks can be conducted across state lines.
How Could the IMLC Benefit Telemedicine?
According to mHealthIntelligence, more than 500 clinicians have obtained an average of two licenses since the process opened in 2017. It’s an expedited process that physicians with a telehealth practice can make use of.
Today, one of the challenges of providing care to our mobile population is that, if your patient goes to Florida on vacation and comes up sick, you cannot treat them via a telemedicine app without being licensed in that state. But there are other determining factors that vary by state to consider. So, while having state medical boards serve an important function around licensure, they do seem to complicate the process of providing telemedicine. But there are signs everywhere that the barriers to telehealth are lifting.
The IMLC is not without its problems, certainly, but it should be noted that it is just the first attempt at creating a universal standard that could facilitate telehealth applications over time. The Patient Safety & Quality Healthcare (PSQH) stated:
While one can argue both sides of the “states vs. federal” regulation question for medical boards, as it stands, each state has a huge say in who can practice medicine within its borders. And each state has its own “physician lobby” that has no interest in giving up control of state medical licensure laws.
Politics aside, the concept of the IMLC is in its infancy. As the government continues to loosen originating site restrictions, which was one of the original barriers to telehealth, isn’t it possible that the IMLC also will continue to revamp their process to boost the adoption of telehealth technology?
OrthoLive providers and other clinical teams using telehealth will benefit as the barriers to using this technology continue to fall away. The OrthoLive telemedicine product allows orthopedic specialty providers to extend care into rural communities where there are no orthopedists available. Telehealth can help improve care continuity while cutting costs. These are just a few of the benefits.
Contact us to find out more about going live with telehealth in your practice.



