 Telemedicine is widely used by hospitals and health systems across the United States to improve access to care. For those researching the technology, note that there are three primary phrases used interchangeably to describe similar technologies.
Telemedicine is widely used by hospitals and health systems across the United States to improve access to care. For those researching the technology, note that there are three primary phrases used interchangeably to describe similar technologies.
What is Telehealth?
The overarching category that telemedicine and e-Health fall into is generally considered “Telehealth.” A March 2018 white paper called “The Promise of Telehealth: Strategies to Increase Access to Quality Healthcare in Rural America” defines telehealth as, “communication and information technologies used to provide or support long-distance clinical healthcare, patient and professional health-related education, public health, and health administration.”
The Center for Connected Health Policy says, “Telehealth encompasses a broad variety of technologies and tactics to deliver virtual medical, health, and education services. Telehealth is not a specific service, but a collection of means to enhance care and education delivery.”
Part of the problem here is that federal and state agencies differ in how they define these applications. For example, California law says:
“The mode of delivering health care services and public health via information and communication technologies to facilitate the diagnosis, consultation, treatment, education, care management, and self-management of a patient’s health care while the patient is at the originating site and the health care provider is at a distant site. Telehealth facilitates patient self-management and caregiver support for patients and includes synchronous interactions and asynchronous store and forward transfers.”
But the federal Health Resources & Services Administration says:
Telehealth is defined as the use of electronic information and telecommunication technologies to support and promote long-distance clinical health care, patient and professional health-related education, public health and health administration.
Generally, telehealth encompasses the following technologies:
- Live video, or synchronous (two-way) virtual visits between a person and their caregiver using telecommunications technology.
- Store-and-forward, or asynchronous virtual visits that do not include the use of live feed, but instead use pre-recorded videos or digital images and the Internet to transmit this data.
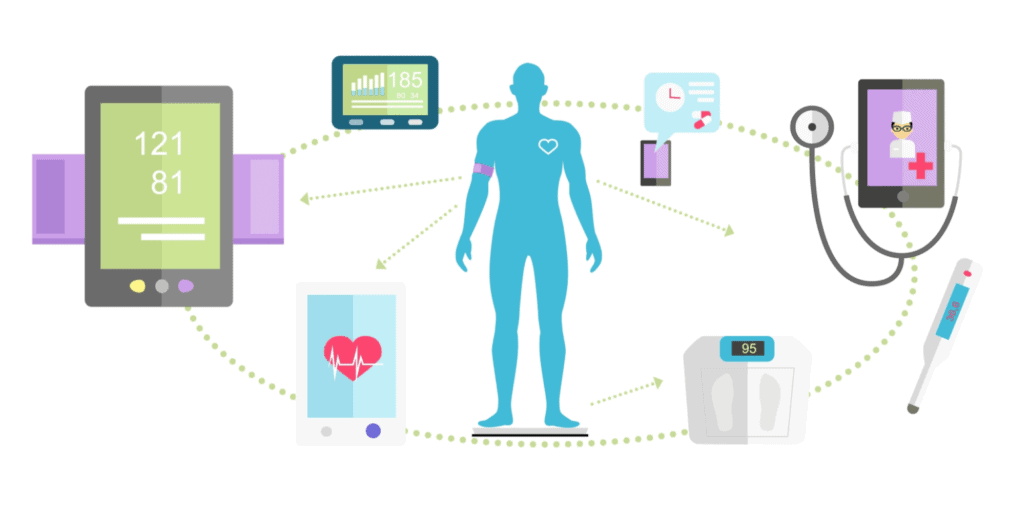
- Remote patient monitoring includes a patient sensor or another on-site machine that transmits information virtually through the web to a remote caregiver.
- Mobile health, often called mHealth or eHealth, is a virtual visit conducted via a cell phone or other digital handheld devices like a PDA or tablet and not on a desktop.
While these generally are the four categories that are widely recognized in the industry, some technologists also list a fifth category called “eConsult,” which uses telehealth technology to transmit clinical data between two medical providers, such as a primary care doctor and a specialist. An eConsult can consist of just the transmission of data (store-and-forward) or real-time video consultations (synchronous telehealth). The distinction between synchronous visits and eConsult is that the communication is not between doctor and patient but two consulting clinicians.
No matter how the sub-categories are defined, telehealth is the framework for a technology that allows communication between two (or more) individuals within a healthcare setting. This may or may not include clinical visits, patient education, or some other type of remote monitoring process.
What is Telemedicine?
If telehealth is defined as the overarching services framework, where does telemedicine fit in?
The Center for Connected Health Policy suggests the concept of telemedicine is slowly being replaced by the more commonly used phrase “telehealth.” While we’re not certain that is necessarily true in many medical circles, there is consensus that telemedicine refers to the practiceof using telehealth technology for medical applications.
However, the American Telemedicine Association (ATA) defines telemedicine as:
In brief, telemedicine is the remote delivery of health care services and clinical information using telecommunications technology. This includes a wide array of clinical services using internet, wireless, satellite and telephone media.
The ATA uses telehealth and telemedicine as interchangeable terms, which supports the general usage of the two phrases as synonyms. Generally, across the industry, telemedicine and telehealth are considered to be remote or virtual healthcare technology to deliver care to patients.
How Does e-Health Differ from Telehealth and Telemedicine?
E-Health was defined in a clinical study as far back as 2001 in the Journal of Medical Internet Research. In the research paper, the authors suggest that e-Health actually signifies a broadening of the telehealth category to integrate the technologies as a standard part of treatment. The authors suggested that when e-Health is broadly adopted as a descriptor for telemedicine applications, the technology will have reached widespread adoption in a similar way as e-commerce applications have become normalized in the retail sector. The article suggested the phrase was “an umbrella term…to describe the combined use of electronic communication and information technology in the health sector.”
Ironically, even health systems have their own definitions of these phrases. For example, The University of Kansas Medical Center says e-Health “refers to the use of computers and networks like the Internet to store and manage your medical records, instead of paper files.” They use this term interchangeably with the phrase “health information technology” (HIT).
Even educators are split on how to use these terms; Jacksonville University says, “eHealth is where medicine/healthcare and information technology converge.” They define forms of eHealth as:
- Health informatics (HIT) for digital management of patient records.
- Telemedicine to facilitate remote diagnoses and clinical care.
- Electronic health records (EHR), a form of HIT.
- Clinical decision support systems, which provide digital access to protocols to improve quality outcomes.
- Consumer health informatics, which includes smart digital devices to monitor exercise, weight, eating habits, and more.
Science Direct also includes the application of health interoperability between data exchanges, such as Health Information Exchanges (HIE) under the eHealth banner. HIE networks include the Department of Veterans Affairs, who has a long and successful history of applying telemedicine to improve access to care for our nation’s veterans.
OrthoLive is Telemedicine
No matter the definition you select, it’s clear that telehealth technology is evolving into more widespread use by hospitals, medical practices, payers, and employers.
OrthoLive has a telemedicine application that allows orthopedists to better connect with their patients. The application works on any digital device and is offered as a low-cost subscription service that can apply telemedicine to any orthopedic workflow. It has a convenient mobile health (mHealth) component but also functions well on any tablet or desktop computer. Contact the OrthoLive team to find out more about this service and how it could help your patients and your practice.



