 Many doctors consider telemedicine as something new, a strange and unfamiliar way of interacting with their patients via a video screen. In fact, studies show that the slow adoption of telemedicine in the medical practice has been fueled by the reluctance of the physicians themselves to adapt to the technology.
Many doctors consider telemedicine as something new, a strange and unfamiliar way of interacting with their patients via a video screen. In fact, studies show that the slow adoption of telemedicine in the medical practice has been fueled by the reluctance of the physicians themselves to adapt to the technology.
What these slow adopters may not recognize is, despite their discomfort with telemedicine workflows in their practice this technology has been around since the 1950s. Over time, as the Internet and our software and hardware have improved, we’ve found more effective ways to apply this technology in healthcare settings. The years have brought us a plethora of data proving the efficacy of telehealth to improve quality, convenience, and cost in medicine.
So what is the history of telemedicine? Where did the technology start and how has it been used? What are outcomes telling us about the use of telemedicine in the medical practice? This article will review the facts.
Telemedicine – An Old Idea in Modern Packaging
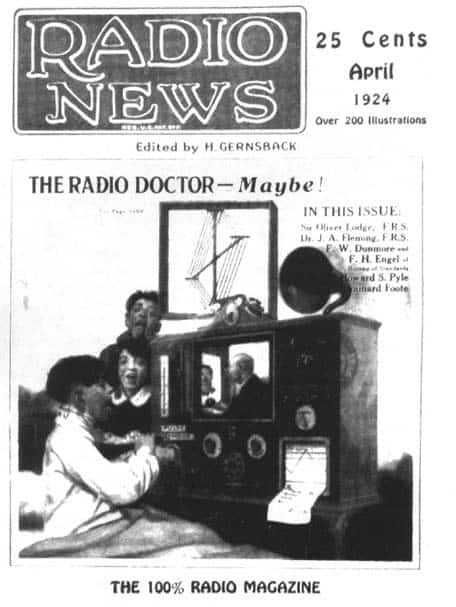
Telemedicine was perhaps first conceived in 1924 when the black and white cover of Radio News showed a doctor conducting a patient encounter via a radio transmission. It took nearly two more decades for this groundbreaking sci-fi idea to become reality.
(Graphic from Telemedicine: A Guide to Assessing Telecommunications in Health Care. Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine; Field MJ, editor.Washington (DC): National Academies Press (US); 1996.)
By 1950, radiologic images began traveling back and forth between physicians via the phone lines. This groundbreaking work happened in Pennsylvania, USA, but Canadian radiologists developed what was the first teleradiology system later that decade. Using television to transmit patient data in diagnostic radiology was one of the first applications in telemedicine, but some of the other early efforts at telehealth included:
- Using coaxial cable to transmit telefluoroscopic examinations.
- Ship-to-shore transmissions of EKG and x-ray data.
- Using voice radio channels to transmit EKG rhythms from a remote location to a hospital.
- Using an interactive television microwave link to transmit voice, EKG, microscopy, and other clinical data.
Ironically, the textbook, Telemedicine: A Guide to Assessing Telecommunications in Health Care, says these types of transmissions “are now so routine and so much a part of mainstream health care that they are often not mentioned as telemedicine applications.”
NASA was an early pioneer of telemedicine; the Harvard Business Review (HBR) recently chronicled their work over the past five decades. The article noted that the use of telemedicine is critical to space travelers where the gravity-free environment affects bone, muscle, fluid distribution, and immunity. HBR suggests that the use of telehealth in space can provide us with important data “to improve care in other remote, extreme, or otherwise resource-constrained environments.”
According to Telemedicine: A Guide to Assessing Telecommunications in Health Care, by the 60s and 70s some of the biggest names in healthcare joined NASA in experimenting with these early telehealth applications in a variety of specialty care settings:
- Massachusetts General Hospital was communicating medical treatment data remotely to nurses in emergent medical situations at Boston Logan Airport.
- The Veterans Administration Hospital and Massachusetts General established a telepsychiatry practice.
- The Mt. Sinai School of Medicine used telehealth to supervise midlevels in ambulatory care clinics.
All of these trials and errors set the stage for what was to become the biggest disruptor of every industry in every country: the Internet.
Telemedicine Today and the Impact on Healthcare Outcomes
“The number of telemedicine users is now expanding rapidly enough that no complete inventory of applications is available, especially for projects involving private nonprofit and commercial sponsorship or funding.”
Telemedicine: A Guide to Assessing Telecommunications in Health Care
In the last fifty years, telemedicine has moved into the mainstream. If you want to realize how far the technology has come, consider that in 2016, Kaiser Permanente announced they were seeing more patients in virtual telehealth visits than they were via traditional in-person visits.
The milestone was picked up in mhealthintelligence, who noted Kaiser’s powerhouse status in healthcare; the California health system treats more than 110 million patients annually. But in 2016, 59 million people connected virtually via apps, web portals, and virtual visits.
It was a breakout year for telemedicine, clearly establishing the technologies growth into mainstream healthcare. The article stated it was the first year that a large health system reported virtual encounters surpassed traditional visits. From 2014 to 2015 Kaiser used telehealth applications in the following ways:
- Sent 20 million emails between patients and their doctors.
- Scheduled four million appointments.
- Viewed 37 million tests online.
- Refilled 17 million patient prescriptions.
But this is just one, albeit huge example of the mainstreaming of telehealth. As a milestone, it signaled to the wider healthcare community that telehealth is both a legitimate form of patient care and a secure technology.
Becker’s Hospital Review says, “Telehealth can benefit nearly 80-plus specialties – including neurology, radiology, dermatology, pediatrics, psychiatry and chronic disease management.” A 2018 AARP article provided some examples of how telemedicine is being applied today in a variety of clinical settings, including:
- Clinical trials have shown remote patient monitoring, a form of telehealth, improved the treatment regimen for chronically ill cardiac patients. Remote daily monitoring of weight, diet, physical activity, medication compliance, and stress management has been shown to improve outcomes in these patients.
- Studies show telehealth improves diabetes management by educating and engaging patients. Chronic diabetes sufferers’ benefit from daily care and monitoring of glucose levels, blood pressure, weight, and other health data. It enables clinicians to better adjust treatment protocols in order to proactively treat their patients.
- Telemedicine is being used today to provide home care to the elderly and sickest populations. As the Baby Boomers age, telehealth applications will play an increasing role in linking specialists and primary care providers with patients that are no longer mobile and for whom an in-person traditional visit would be a real physical hardship.
The benefits of virtual visits for patients are that they reduce the burden of travel and time off work. Too, these visits provide care in regions where no clinician is located, expanding access to care. For clinicians, telemedicine offers a way to stretch the bottom line while still providing the best care to any selected population.
Today, after more than five decades, telehealth has become an accepted part of the majority of health systems across the United States. This proven, established technology is an important part of the future state of healthcare both in the United States and abroad.
OrthoLive is proud to be a part of telemedicine’s evolution. Contact us to find out more.



